We hope you find some of these tips useful. This section will continue to grow as people send us their tips.
For people with a learning disability.
Where possible we include links to information designed for people with a learning disability. These are usually 'easy read' so can be read by the person with the learning disability or be used by their carer, friend or family member to explain cancer and cancer screening to them. These resources all come from, or are endorsed by, reliable sources like Public Health England, NHS Trusts etc.
For children.
Where possible we include links to information designed for various stages of childhood. These resources all come from, or are endorsed by, reliable sources like Public Health England, NHS Trusts etc.
Self-Awareness / Self-Examination
It is important that everyone, regardless of gender, checks regularly for any changes in their breasts. This ensures that they know their breasts well and are more likely to spot any changes.
There are two types of breast-self-exam. Which one you should do depends on your body type. They can be found below.
If you already have scans due to your age, genetics or an existing cancer you should still do regular self-exams. The sooner cancer is found the better the prognosis.
Any changes you notice should be checked by your GP. If you are already a cancer patient then it may be more appropriate to check with you Breast Nurse or your Oncology team.
Breast Self-Exam Type 1
This type of exam applies to:
- women;
- gender non-conforming individuals born female;
- transgender men who have not had top surgery (mastectomy).
N.B. Excessive testosterone can be converted to oestrogen and increase the cancer risk for transgender men.
This image from the Know Your Lemons Foundation captures the changes people in the above groups should look for in their breasts.

cancer.JE note - For a dimple to form in your breast you will first have a slight flattening of that part of your breast. When doing your self-exam moving a mirror around your breast can help you identify any flatter areas.
Breast Self-Exam Type 2
This type of exam applies to:
- men;
- gender non-conforming individuals born male;
- transgender men who have had top surgery (mastectomy).
N.B. Top surgery may not have removed all of the breast tissue.
While breast cancer is far less common for people in the above groups they can still develop it. The list below indicates what symptoms to check for.
Symptoms
- lump in the breast
- nipple discharge
- swelling of the chest area
- lump or swelling in the underarm
- rash or sores on the chest or nipple area
- inverted nipple (the nipple pulls in towards the breast)
Breasts can change during puberty as testosterone production increases, and with ageing as testosterone production lowers.
Screening Programmes
Jersey has three cancer screening programmes, please see below for more information.
For people with a learning disability
In each section we link to a booklet from NHS England. These booklets are designed so that they can either be read by people with a learning disability or for their carer, friend or family member to use to help explain the screening to them. N.B. Due to these booklets being intended for patients in England and Wales while most of the advice will be suitable for Jersey there may be some information specific to England and Wales.
Bowel Cancer
Official information on bowel cancer screening can be found at the Government of Jersey's Bowel Cancer Screening page.
Bowel Cancer Screening information for those with a learning disability.
Breast Cancer
Official information on breast cancer screening can be found on the Government of Jersey's Breast Cancer Screening page.
Breast Cancer Screening information for those with a learning disability.
Cervical Cancer
Official information on cervical cancer screening can be found on the Government of Jersey's Cervical Cancer Screening page.
Cervical Cancer Screening information for those with a learning disability.
Vaccinations
HPV (Human Papillomavirus) Vaccine
This vaccine can stop people getting some forms of HPV. This decreases their chances of developing a number of types of cancer including those of the head and neck.
The vaccine is:
- offered at school to children aged 12/13;
- given as 2 injections 6 months apart;
- offered to all genders.
The vaccine doesn't protect against all types of HPV. It is important that people with a cervix still attend for cervical screening. This can include some transgender men.
Official information on the HPV vaccine can be found on the Government of Jersey's HPV vaccination page.
Genetics - coming soon!
Transgender & Gender Non-Conforming People
Periodically news broadcasts report on healthcare inequality for transgender people. We hope things are improving. But we realise cancer won't wait for things to improve.
We encourage everyone to make sure the right screening programmes are available to them. We also encourage everyone to take part in those screening programmes. This will enable the earliest possible diagnosis and best prognosis.
Below are some matters you may want to consider and check. If you notice any worrying symptoms please do not hesitate to check these with your GP. If these symptoms cause you distress relating to your gender support is available. We recommend seeking support from Liberate. Liberate offer support to transgender and gender non-conforming islanders.
If you are 25 or younger then the Youth Enquiry Service (YES) offer counselling. The service is free and confidential. Counsellors have experience of working with LGBT+ young people.
Cancer Screening Programmes
Which screening programmes you are invited to may depend on what gender you are registered as with your GP. Please check with your GP that you will be invited for the appropriate types of cancer screening. Remember that if you undergo gender reassignment surgery or hormone treatment you may need to reassess your cancer risk and screening options.
Breast Cancer
In our Self-Awareness/Self-Examination Section there is information on the two different types of breast exams. Please use whichever one most closely fits with your current physical body.
Cervical Cancer
We would like to remind pre-GRS transgender men that they should still have cervical smear tests. Cervical smear tests are for anyone with a cervix who is aged 25 to 64, no matter their gender.
Testicular Cancer
We would like to remind pre-GRS transgender women that they should carry out self-exams on their testicles. Anyone with testicles should do testicular self-exams, no matter their gender. Post-GRS transgender women are not at risk of testicular cancer.
Bowel Cancer
Coming soon!
Radiology
Official information can be found on Jersey General Hospital's Radiology page. It includes a video that shows what to expect on arrival at the department.
Radiation Safety
Jersey General Hospital offer useful information on radiation safety on their Radiation Safety page.
Biopsy
NHS Inform (NHS Scotland) have general information on biopsies as well as information on the different types of biopsies.
Jersey General Hospital have a small section about biopsies on their Interventional Studies - Radiology page.
CT (computerised tomography)
Official information can be found on Jersey General Hospital's CT (Computerised Tomography) page. It includes a video showing what you can expect at your appointment.
Mammogram
Official information can be found on Jersey General Hospital's Mammography page. It includes a video showing what you can expect at your appointment.
Unless you already have pain or tenderness around the area being scanned the mammogram shouldn't hurt. It can feel uncomfortable for some and it does involve pressure on the chest, but it doesn't take long and staff will help put you at ease and answer any questions you have about the process.
MRI (magnetic resonance imaging)
Official information can be found on Jersey General Hospital's MRI Scans page. It includes a video showing what you can expect at your appointment.
Scans - with Contrast
Sometimes a scan appointment will be for a scan with contrast.
At least one of the types of contrast dye has an interesting but very short-lived side effect. Which is that it can make make someone feel like they have wet themself. They haven't!
Some patients report feeling a warmth flood over them and move down their body from head to toe. Others only feel that warmth in their pelvic area. Others feel something in between. If the sensation is just in the pelvic area it really can feel like wetting oneself. It's not the best feeling if this is a scan for which you had to drink lots of fluid first.
The Radiologist will warn you about this beforehand. Of course they may not actually have experienced it themselves. As patients we can assure you that they mean what they say!
Ultrasound
Official information can be found on Jersey General Hospital's Ultrasound page. It includes a video showing what you can expect at your appointment.
X-Ray
Official information can be found on Jersey General Hospital's X-Ray Scans page. It includes a video showing what you can expect at your appointment.
First Things First
Sorry if you find yourself here having just been diagnosed with a form of cancer. We wish you all the best with your treatment and hope you find some of these tips to be of help.
A diagnosis of cancer often comes with an overwhelming amount of information. For this reason we recommend only reading the sections of this site that could be helpful to you right now. Come back to the other sections as and when they are relevant to you.
Here is our cancer patient's beginner guide.
- Stop and take some deep breaths. Repeat as necessary.
- Don't waste time wondering "why me?" or blaming yourself for lifestyle choices. Cancer can hit anyone at any time. In the majority of cases it is impossible to determine what caused an individual's cancer. Some health fanatics die young from cancer. Yet other people lead a very unhealthy lifestyle and live to old age without getting cancer.
- Dr. Google brings up more wrong information than it does helpful information. The best source of information is your Oncology team. They are the only people that know the specifics of your cancer. If, however, you do search online it is best to look at reputable Jersey and UK websites. See the section Information on Cancer for links to reliable and comprehensive information.
- Whatever you are feeling, even if it is anger, is okay. Don't beat yourself up about it.
- You may experience a range of emotions in a short space of time.
- No matter how independent you are you will need support.
- Take someone with you to every appointment, at least initially. With cancer on your mind it's easy to lose some of your focus. Cancers are complex diseases so a second set of ears is useful.
- When you have an appointment pending it can be helpful to write down questions you expect to ask. Then take the list with you so you don't forget them.
As fellow cancer patients we can tell you that the time between diagnosis and starting treatment is one of the hardest times we faced. It is common to feel as if treatment isn't starting soon enough and to feel frustrated. We assure you that life begins to settle once your treatment, or surgical plan, is underway.
Here are our tips for once your diagnosis has sunk in.
- Once you have time to stop and think check if you have Critical Illness Cover. If you do then check whether your specific cancer is covered.
- Start a Health Diary. Through your treatment you will often be asked questions about allergies, surgeries, medications etc. Inevitably there comes a stage where you forget to mention things. See our section 'Health Diary'.
- Make sure you are aware of any health benefits/schemes your workplace offers. Remember a family member may have a workplace scheme that provides for you.
N.B. Most people donate to cancer charities at some point in their lifetime. And they do so because they want the support to be there for people in their time of need. If you are now the one in need please take the support, others donated so it would be there for you!
Emotional Support
At every stage of your cancer experience emotional support is available in a variety of different forms.
In a Crisis
If you find yourself in crisis please contact your GP or the Samaritans.
For out of hours GP services contact JDOC.
For the Samaritans.
It can be very useful to keep the numbers for these organisations in your phone so that they are readily accessible should you need them.
Face to Face
For Face to Face support we thoroughly recommend Macmillan Cancer Support Jersey. They offer emotional support and counselling.
We also recommend the Listening Lounge for counselling.
Online
In January 2025 the Centre for Psychosocial Research in Cancer (CentRIC+), part of the University of Southampton, launched a fantastic website to guide people through emotional support at every stage of their cancer experience.
CAN-EMPOWER ™
Please note that the links for support are all UK-based. Should you require support here in Jersey you can find local options mentioned throughout our site.
Taking Control
That feeling of loss of control can be what leads people to seek out alternative treatment. Yet using alternative treatment lowers your chance of survival. Thankfully there are much safer ways to regain a sense of control over your life.
For many types of treatment it is a good idea to do the following before it starts. N.B. These tips may not be suitable for someone with your type of cancer, please check with your medical team first.
- Have a dental check-up.
- If possible, have any necessary dental work carried out before starting treatment.
- Increase your dental hygiene routine to keep your gums as healthy as possible. Gum problems are one of the easiest ways for you to get an infection due to having many bacteria in your mouth.
- Moisturise your skin morning and night. Pay particular attention to your hands and feet. Cracks in your skin are one of the easiest ways for you to get an infection due to having bacteria on your skin.
- If you don't have an exercise regime you could start one. Exercise is beneficial during treatment. The fitter you are before treatment the easier it will be to exercise during treatment. Check The Directory to see if there is any exercise support available to you.
- Some people choose to adopt a healthier diet. A healthy diet is always a good idea but what is healthy varies from person to person. For a cancer patient what is healthy also depends on the type of cancer. It is important to get advice from a medical professional who knows your specific cancer. Speak to your medical team for advice. Macmillan Jersey also have a Dietitian that specialises in cancer, you can contact them through the Macmillan Jersey website.
- Once you know what type of treatment you will be having you can check the relevant tips on this page and plan for it.
Information on Cancer
Cancer is the umbrella term used for more than 100 related, but different, diseases. What they have in common is abnormal cell growth. Other than that they differ a lot.
Each human's cells are unique to them. And so the cancer that develops from those cells is also unique to them. Even two cancers of the same type will differ from each other.
When looking for information on cancer always check that the information relates to your type of cancer.
Below we offer links to trustworthy and useful websites for information on cancer.
Information from Charities
Leaflets/Books
At Macmillan Jersey's drop-in centre (The Oasis) there is a large bookshelf full of information on different cancers.
Online Information
Both the UK charity websites offer lots of information covering the majority of cancers.
N.B. Bear in mind that some information, especially if about charity services or health services, may not be relevant to Jersey.
Public Healthcare Systems
- NHS Inform - NHS Scotland
- A to Z of Conditions - NHS England
Both these sites offer lots of information on different cancers.
N.B. Bear in mind that some information, especially if about healthcare services, may not be relevant to Jersey.
Telling Other Adults
Some things our tip contributors learned.
- It's easy to underestimate how tiring telling people is. You may need some time to rest between telling people.
- You might want to tell a small number of people and specifically ask them to break the news to other family or mutual friends.
- At the time of breaking the news you will probably not know much about your cancer or your treatment plan. People who haven't had cancer might not realise how little you know. So it can be helpful to be clear at the outset that you are telling them all you know. It can save you from facing lots of questions you can't answer.
- No matter who you are you cannot do this alone, you will need support from at least one other person.
- The person you confide in may struggle with the news. It may help to allow them to discuss it with one another person. This could be someone you can also trust, or someone you don't know at all.
- If you tell people over the phone, are they alone? Do they have someone for comfort once the call ends?
- Everyone has their own perception of cancer. This can come from media portrayal of cancer or from personal experience. Their perception will often be far removed from what you are going through. Experiences vary a lot from one cancer patient to another.
- It is likely that people who know you will discover in time that you have cancer. For this reason it might be better if they hear it from you so that you get to 'write the story'.
- Telling people face to face, or over video-link, can have some benefits as they can see how you are.
- Cancer is very common but people still struggle with what to say to cancer patients. You may have to dig the depths of your patience levels. It's okay if you can't though, you have enough to deal with!
Incurable/Inoperable Cancer
Understanding your situation does not mean you have given up. Nor does it change your life expectancy. Understanding your situation can help you live your best life.
Telling Children
Below are some resources that can help you talk to children about what is happening to you.
- The Little C Club card pack - For children aged 2 to 10. Designed by a nurse and a design teacher, who also happened to be cancer patients. Borrow from us - we have a pack which you are welcome to borrow. Should you wish to borrow it please just email salut@cancer.je.
- My Parent Has Cancer And It Really Sucks book (American) - For children aged 12 to 17. Compiled by a teenage girl (whose mum had breast cancer) and her father, incorporating advice from medical professionals and real stories from 100 teens. You teenage will really know they are not alone. Borrow from us - we have this book which you are welcome to borrow. Should you wish to borrow it please just email salut@cancer.je.
- Talking To Kids About Cancer by the Cancer Council (Australia) - (Download pdf Booklet) - For children aged from birth to 18. This is a fantastic online resource that explains the understanding children have of cancer at different stages in childhood, as well as the understanding they have of death at those different stages. It offers help with the best wording to use, what wording to avoid (so you don't make the child fear normal life experiences), a glossary for common cancer terminology and how to explain it to different ages of children, and ideas of activities you can do to help a child understand what you are going through.
N.B. For the two non-British resources bear in mind that some terminology may differ. We include them because overall they are fantastic resources.
First Oncology Appointment
Depending on your type and stage of cancer, as well as your treatment plan, you will find yourself speaking either to a Surgeon or an Oncologist. Here are some tips and information if you have to see an Oncologist.
- Your first meeting will usually be with an Oncologist and a Cancer Nurse Specialist.
- In most cases the first appointment will involve discussion, not treatment.
- Ahead of your appointment start thinking what questions you might want to ask. Write these down and take the list with you.
- Your oncologist will give you an idea of what will happen next. This often involves scans and further tests to stage your cancer.
- Your oncologist may give you an idea of what your treatment plan is likely to be. Be aware that this plan may change as the results of further tests are received and analysed. Information from the various tests helps guide your Oncologist to the best treatment for you.
- There can be quite some time, even many weeks, between diagnosis and starting treatment. This can be frustrating for the patient. But it is important for your Oncologist to get as much information on your specific cancer as possible. This information helps them choose the best treatment for you. Do not panic. If a delay in treatment could have a negative effect on your prognosis then treatment will be started while they wait for test results to come in. This just means that your treatment may be changed once your test results are in.
- The nurse will take time with you to go over your treatment plan and show you around the treatment bay. They will also have you sign documents agreeing to treatment. They will not rush you and you can ask any questions you have.
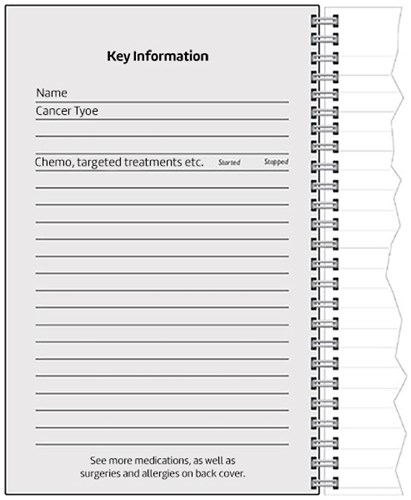
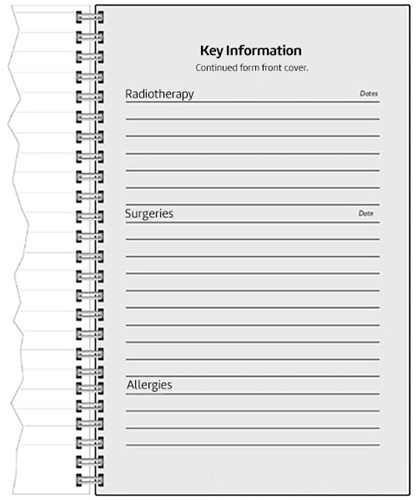
Health Diary
With cancer you can find yourself often having to state your surgeries, chemo, medications, allergies etc. If, and when, that list increases inevitably you end up forgetting to mention things.
Also, you may be given medications to take "as and when required". If you have to see a doctor and they ask "What have you taken today?" those are easy to forget.
If you develop side effects your oncologist will want to know when they happened, how intense they were etc.
At a time in your life where your brain is flooded with information your doctors need you to remember tiny details of life since they last saw you.
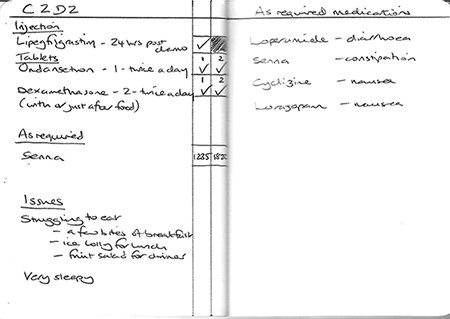
So we recommend keeping a health diary from the moment you start treatment. Our founder kept one, and gives a rough idea of it in the images below.
Here is a list of what you might consider keeping a note of in a prominent place, like the front and back covers.
- Your exact diagnosis (including stage, grade, receptors etc.).
- Chemotherapy & targeted treatments, listed with start and stop dates.
- Medications, both those you have to take, and those you take "as required". You will sometimes be asked the dose and frequency. It can also be helpful to write what each "as required" medication is for. (Remember to include medications you take for other conditions.)
- Radiotherapy, including dates.
- Surgeries, it can help to use the proper name of the surgery, including dates.
- Any allergies you have.
- Other significant conditions you have.
Here is some information you might consider keeping within the body of the notebook.
- Mark each page by day, according to your treatment. So for chemotherapy you can have C1-D1 (cycle 1, day 1) and so on, along with the actual date. If you need to call the On-Call Oncology line you will likely be asked where you are in your chemo cycle.
- You can pre-fill in what drugs you need to take on each day. How you are to take them. And have boxes to tick when you do take them.
- For drugs taken "as required" you can mark in the boxes the time you took them.
- Any symptoms you had that day. It's helpful to record what you were doing at the time. What had you eaten? Were you sitting, standing, lying down etc.? Whatever might be relevant to the symptom.
- If you are struggling to eat it can sometimes be of use to keep a note of what you are eating. This can help your Oncologist assess how you are getting on.
Genetic Testing - coming soon!
Vaccinations
Some cancer patients assume they are unable to have vaccinations. This isn't true. Vaccinations may be recommended for your specific situation.
You may be used to not worrying about viruses. But certain treatments put you at increased risk of severe illness, even death, if you get a virus. Certain treatments make vaccinations less effective. So even with vaccination your risk of harm may still be increased. It may be advisable for your household to be vaccinated to help protect you.
Our advice is:
- ask your Oncologist if there are any vaccinations you should have;
- ask if there is a specific time when you should have it (eg. before treatment begins);
- ask if they recommend those in your household are also vaccinated.
We would recommend asking specifically about the flu, pneumonia, and COVID-19 vaccines.
Meeting Other Cancer Patients
It can be beneficial to meet and talk to other cancer patients. Even if you know people who have had cancer in the past. There is something helpful in talking to a person who is going through it all at the same time as you.
Thankfully it's rarely like how TV shows present 'self-help' groups. There are benefits in talking to someone who is going through the same thing. Some things you don't need to discuss because you know they 'get it'. And they are less likely to feel uncomfortable laughing about some of your experiences. Cancer can create some humorous moments after all.
Physical Chats
Various charities in Jersey host social events. You can search for these in The Directory.
Virtual Chats
Below are links to some trustworthy online communities.
Jersey
This fast-growing Facebook group was started by Macmillan Cancer Support Jersey in January 2021.
UK (open to Jersey patients)
Both these online communities have general chat areas, and areas specific to certain cancers and stages. They are well-moderated with a mix of trained moderators and nurses. This ensures they are safe places for cancer patients.
They can be particularly useful if you find yourself struggling late at night. Due to the large number of users there is usually someone on late at night.
The Internet, Social Media & Cancer
The Internet & Cancer
The internet is both a friend and foe to cancer patients.
There are many companies, and individuals, looking to prey on the vulnerability of cancer patients. They see cancer patients as an easy source of money. They hope some people feel so desperate they will readily pay for fake cures and useless products.
Having cancer is expensive. So we advise being very cautious before parting with your money. For far too many of the products targeted at cancer patients there is no evidence that they make any difference.
Our advice to those looking for support or products:
- speak to your Clinical Nurse Specialist or an Oncology Nurse;
- speak to local cancer charities;
- check out reputable UK cancer charity websites like Macmillan UK or Cancer Research UK;
- just because a doctor or nurse uses a product, does not mean it is proven to work;
- cancer patients might claim something worked for them, but be cautious about these claims, especially for products like shampoos (see next bullet point);
- when a patient claims a shampoo helped their hair grow faster and thicker the problem is they have no idea how fast or thick their hair would have grown without that shampoo, they are assuming it grew faster and thicker, they don't actually know, the only way to know is to use said shampoo on just one half of your head and compare the results, but no-one does this;
- remember that companies often 'create' a problem so they can then sell a product that claims to solve it, they create the insecurity that we might have about our appearance and then target us with products to allegedly make us look better and be more confident.
As stated above, other patients may also be able to offer advice. But be cautious when seeking advice from anyone who is not a cancer specialist. Cancer patients vary greatly. Not just in terms of their cancer. But also in terms of their views. Our founder was targeted by a cancer patient looking to sell her a very expensive but completely useless product.Social Media & Cancer
When someone mentions cancer on social media the software's algorithm pick up on it. The user might then be targeted with dodgy adverts for unproven treatments and therapies.
Example: Mentioning hair loss may lead to being targeted with unproven products claiming to speed up regrowth.
Our advice is to completely ignore adverts. It is safest to check with your Oncology team, or reputable cancer charities, to see what help is available. You don't need to be targeted by products, if you have a problem for which you want a solution you are perfectly capable of looking for the solution yourself.
Alternative Treatment
We have a whole page dedicated to Alternative Treament, please check it out.
Surgery - coming soon!
Chemotherapy
If you know that you are likely to be starting chemotherapy then there are some useful things you can do now. This can help you feel like you have some control over your situation.
- Arrange a check-up with your dentist as a matter of urgency.
- Have any necessary dental work carried out before starting chemotherapy.
- Increase your dental hygiene routine to keep your gums as healthy as possible. Gum problems are one of the easiest ways for you to get an infection due to having many bacteria in your mouth.
- Ensure your daily fluid intake is good, if not then increase it.
- Moisturise your skin morning and night, paying particular attention to your hands and feet. Cracks in your skin are one of the easiest ways for you to get an infection due to having bacteria on your skin.
- Although you may feel able to drive to chemotherapy it is best to get a lift as you may not be able to drive yourself home. Over time you will get to know what is possible for you.
- Once treatment is under way you might want to prepare a 'Go Bag'. You may not need it but if you have a sudden admittance to hospital it makes it easier for someone else to bring in what you need. See section # for tips on what you might include.
- Chemotherapy can mean many hours in the Oncology Treatment Bay. Some treatments take under and hour, others can take all day. See section # about the treatment bay.
- Constipation is a very common side effect of chemotherapy. See section # on constipation for tips.
- Eating can become more complicated when you are on chemotherapy. See section # for tips related to food and drink.
See our section 'Cancer Drugs' for links to reliable information on the various drugs used to treat cancer.
Cancer Drugs
Information On Drugs
Various drugs are used to treat cancer including chemotherapies, immunotherapies, hormone therapies and targeted drug therapies. Reliable information on these drugs can be found using the links below. Both Cancer Research UK and Macmillan Cancer Support UK's treatment information sheets are written with patients in mind. If you are using the search function on the eMC website then you can filter (left-hand side) to get medicine information for patients. When the search engine list of drugs appears you will see (on the right-hand side) a link to 'Patient Leaflet'.
Please also see our section on 'Reporting Side Effects'.
Oncology Treatment Bay
If you require chemotherapy drugs delivered into a vein then you will be spending some time in the Oncology Treatment Bay. Here is some information about it.
- It is a light airy environment with a pleasant feel to it.
- You will be treated on a large electric chair and you can adapt the chair's position to lie back if you want.
- There is limited access to plug sockets. It is best to charge any electrical equipment before your appointment.
- The wi-fi signal is good and generally copes with most things.
- (Visitors are allowed although there is limited room around each chair.) N.B. Due to COVID-19 visitors are currently only allowed in special circumstances.
- Various teas, coffee, hot water, cold water and biscuits are available for the patient and visitors.
- Soup and sandwiches are available for those patients in treatment over lunchtime.
- There is a spacious disability-friendly toilet room (with shower). There are also two other smaller toilet rooms just outside the Treatment Bay.
- Your reaction to a treatment might be that you feel a bit cold or a bit too hot so wearing layers can be helpful. Blankets are available if you are too chilly.
- If you need to go to the toilet you can unplug the back of the machine and take it with you. But first time this happens it's definitely best to call on one of the nurses.
Radiotherapy
Information for Patients
The charity Radiotherapy UK has an excellent section on its site with information for patients.
Radiotherapy TechniquesDeep Inspiration Breath Hold (DIBH)
It is sometimes referred to as the deep inspiratory breath hold technique.
Radiotherapy.org.uk has further information and a video that talks through the Deep Inspiration Breathhold Technique. The processes used may differ, but the technique itself should be the same.
Treatment Ports and Lines - coming soon!
Reporting Side Effects
To Your Oncology Team
It is important that you report all and any side effects to your Oncologist or the nursing team. This includes those side effects that maybe aren't bothering you as much. Sometimes the side effects that bother the patient the most are the least serious (medically speaking), and vice versa. Ensuring your team know all the side effects you are having can also help put your mind at rest.
The Yellow Card Scheme (inc. herbal and homeopathy remedies)
We encourage you to report the side effects of any medicines and any herbal or homeopathic remedies you take through the Yellow Card Scheme. If you prefer to use the Yellow Card app it can be found at the Apple App Store or the Google Play Store. Both the website and the apps ask you a number of questions which take you stage by stage through the reporting process.
The UK Government have a useful document detailing what information to include in your report, you may wish to have this information to hand before starting the reporting process.
The scheme is run by Medicines and Healthcare products Regulatory Agency (MHRA), an executive agency of the Department of Health and Social Care in the UK. Reports can be an early warning sign of an issue that needs investigating, and can help identify rare side effects. Reports through the Yellow Card scheme are evaluated alongside additional sources of information on that drug.
General Information
- It is possible to receive cancer treatment and have few, even no, side effects.
- The side effects you experience vary from one treatment to another.
- The side effects of a specific treatment differ for each person on that treatment.
- Side effects are often eased by medication. Ensure your Oncologist knows what side effects you are experiencing. Cancer is difficult enough, don't let embarrassment stop you from discussing side effects.
- If side effects are affecting your quality of life, or are harming you, then talk to your Oncologist. They will have a discussion with you about whether they can change your treatment/drug. The decision to change or continue is usually made by the Oncologist and the patient.
- Some side effects decline with regular exercise. Try to stay active, even if you can only manage short walks.
- Psychosomatic side effects will likely get worse if left untreated. This is in contrast to physical side effects. Physical side effects can sometimes remain the same, even decline, when left alone.
- Even for the strongest person there may come a time when the side effects of a treatment are intolerable. It is important to balance treating the cancer with your quality of life. Don't feel bad if you are unable to continue with a type of treatment/drug. It may be difficult to explain to loved ones if you stop a treatment but it is your decision. Should your loved ones ever get cancer their treatment will be their decision.
- All side effects are real, but not all have a physical cause. Those that have a non-physical cause might improve using medication. If they don't then consider other methods of treatment. See our section on 'psychosomatic side effects' for more information.
Breathlessness (Dyspnea)
Complementary Therapy - coming soon!
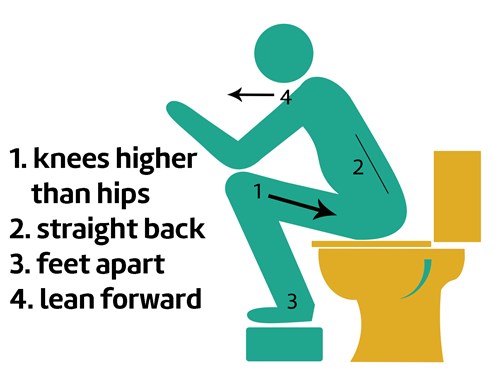
Constipation
Emptying Your Bowels
An NHS guide on Constipation can be found here. It covers the most common causes; treatment and prevention; when to seek medical help; and possible complications. N.B. This NHS advice is not specific to cancer patients. Cancer patients should ensure their Oncology Team are aware of any symptoms they experience.
Treatment
Diarrhoea - coming soon!
Embarrassing Ones
But, what matters is you! The most important thing is that you feel as well as you can at all times. A symptom or side effect may be only a little annoying. But why put up with it for weeks or months when you don't have to? Having cancer is difficult enough, make it as easy on yourself as you can.
No matter what the symptom or side effect is, speak to a professional. That could be a Pharmacist, Nurse, GP or Oncologist. They have heard it all before. They will keep your privacy. They would hate to think you suffered instead of asking for help. Don't suffer over something that is easy to resolve.
Fatigue - coming soon!
Hair & Scalp
If hair loss is likely then going bald, or using wigs and head coverings are all options. Read our sections on Wigs and Head Coverings.
False eyelashes should be approached with caution. The skin around the eyes is already sensitive. And skin can become more sensitive due to treatment.
For those that like to wear makeup Look Good Feel Better events can help.
- What time of year is it? If hair loss is in summer it's important to remember how sensitive the scalp will be to the sun. If it is in winter then body heat can easily be lost through the head.
- How is your scalp? For some people the scalp becomes very sensitive during chemotherapy. This can make the wearing of wigs, in particular, difficult.
See our sections on Wigs and Head Coverings for some ideas.
Cancer patients know that they have a bigger problem to deal with. They also know their hair will grow back. But if, and when, they are struggling they just need comforting.
Head Coverings - coming soon!
Lymphoedema - coming soon!
Mental Wellbeing - coming soon!
Nausea & Vomiting
Nausea and vomiting are the side effects people most associate with cancer treatment. Yet not everyone will experience these. And, if they do, it won't happen with every type of treatment they have. These two symptoms can have a physical cause. They can also be psychosomatic (caused by the subconscious). Please check out our section on psychosomatic side effects.
- If your nausea and vomiting has a physical cause your oncologist can give you medicine to help with this.
- Common home remedies for nausea are ginger and peppermint. These are available in the form of soft drinks, tea, biscuits or sweets.
- 'Mind over matter' can help limit the effects of nausea and vomiting. Example: Repeat "I feel fine" out loud over and over. Do this while taking deep breaths, smiling, and focussing on believing what you are saying.
- Hunger can make feelings of nausea worse. It can be helpful to eat little and often.
- Even short journeys can be difficult if you are vomiting. Keeping medical grade sick bags with you can help give you some freedom back.
- You might struggle to drive during treatment, and not everyone can get a lift to the hospital. If you struggle to get to appointments then contact the Patient Transport Service. You may be eligible for that service.
Psychosomatic Side Effects
Psychosomatic side effects are real. But they are of the brain rather than other parts of our body. Their cause is like that of the well-known placebo effect. If we think something will make us feel better we do feel better. If we think something is going to make us feel bad we do start to feel ill. Society sends out many negative messages about cancer treatment. Our brains have learned to expect nasty side effects.
- If medication isn't controlling your side effects consider that they might be psychosomatic. You can speak to your oncologist about this possibility.
- Psychosomatic side effects range from mild to debilitating. It is important to tackle them as they can interfere with your treatment.
- Psychosomatic side effects will likely get worse if left untreated. This is in contrast to physical side effects. Physical side effects can sometimes remain the same, even decline, when left alone.
- Different medication can sometimes help ease psychosomatic side effects. Speak to your Oncologist about this.
- Alternatively a palliative care doctor may be able to help you manage your psychosomatic side effects.
Skin Conditions - coming soon!
Vaginal Atrophy
Vaginal Atrophy, or Vulvovaginal Atrophy (VVA), is a condition that can affect many aspects of life. It usually occurs after menopause. However, for patients with an oestrogen-driven (oestrogen-positive) cancer the medical and surgical treatments work to minimise oestrogen-production and that can lead to experiencing vaginal atrophy at a younger age. Where Hormone Replacement Therapy (HRT) can help post menopause, it often isn't an option for cancer patients with an oestrogen-driven cancer.
Some of the symptoms of vaginal atrophy are:
- Pain or itching around the vagina;
- Needing to urinate more frequently, burning, urgency or incontinence;
- Pain or discomfort during sex, slight bleeding after sex;
- Recurrent urinary tract infections.
Royal United Hospitals Bath NHS Foundation Trust have a Patient Information Leaflet on vaginal dryness (please note this is a PDF file) and the charity Breast Cancer Now also have a section on vaginal dryness on their website.
The good news is that there are options available to people experiencing vaginal atrophy, even those with an oestrogen-driven cancer. So it is really important to speak to your medical team about any symptoms you are experiencing that could be due to vaginal atrophy.
There are a number of products available to help the symptoms of vaginal atrophy, a selection of these are listed below. N.B. We do not endorse or recommend any products and you must speak to your medical team before trying any products. We only highlight the following to give patients hope and an idea of what is available.
Non-Hormonal Products:
- AH! YES® vaginal moisturisers and lubricants (non-hormonal);
- Hyalofemme® vaginal moisturiser.
Hormonal Products:
- Estriol cream (brands include Ovestin).
Estriol is a hormone replacement therapy cream available on prescription which is suitable for some patients whose cancer is oestrogen-driven. Your oncology team will be able to tell you whether it is safe for you.
Do not suffer vaginal atrophy in silence. Even if you find it embarrassing to raise this topic with your doctor or nurse it is a very brief moment of embarrassment but has the potential to improve your quality of life for years to come.
Wigs
Wigs
There are 2 main types of wig available: synthetic fibre hair and human hair.
- synthetic fibre hair;
- human hair.
There are also enhancers:
- top pieces - of use if you hair has thinned;
- fringe pieces - good for wearing with head scarves.
Friends of Jersey Oncology (FoJO) help pay towards one wig voucher for chemotherapy patients. With that comes information of wig services in Jersey. Dependent on what style of wig you select the voucher may cover the total cost. We give an idea of costs in the sections below. Generally the cost increases with the length of the hair, but not always.
Wigs will come boxed with clear care instructions. Often the makers suggest their own shampoos. It is worth considering what using a normal shampoo will do to the wig. And whether that is an issue for you. It will largely depend on how much you plan on wearing it.
Accessories you might want to buy:
- specific shampoos or very gentle shampoos;
- wig stands - there are ones that fold flat and can be hung up;
- wide-tooth comb (synthetic combs for synthetic wigs).
What to expect with a wig.
- They are a tight fit so wearing them can give you a headache, especially at first. Before reaching for the paracetamol try removing the wig and see if that helps.
- In the summer they can feel very hot, even if you are used to having a thick head of hair.
- Some people find their scalp becomes too sensitive to wear a wig. A cotton wig cap might help if this is the case.
Synthetic wigs
£100 to £300 - Within this piece bracket it is possible to find a good range of wigs. There are all kinds of lengths, styles and colours.
Things to consider:
- requires little or no styling;
- can be cut and styled, but cannot be manipulated as easily as human hair - it's best to use a hairdresser;
- shorter ones have a tendency to look more natural;
- are best cleaned by products specifically for synthetic wigs, but it may be possible to use baby shampoos.
Wigs will always come with care instructions.
Real hair wigs
£500 to £1,500 - Within this piece bracket it is possible to find a good range of wigs. There are all kinds of lengths and styles. Colour is a little more limited, especially for people with auburn hair, but it isn't bad.
Things to consider:
- should be washed before first wearing it;
- is more flexible in terms of styling;
- any cutting or applying of chemicals should be done by a professional;
- are best cleaned by products specifically for synthetic wigs, but it may be possible to use baby shampoos.
Top pieces
Coming soon.
Fringe hair pieces
£20 to £100 - There is a reasonable range of fringe pieces within this price bracket. They can be a good alternative to a wig, especially if you like wearing hats or head scarves. People also use them as a cost-effective way to change their look.
Accessibility
Travel
Jersey does very well with some aspects of accessibility. However, as with most old towns and cities, there are areas that can be challenging for people with reduced mobility.
You can find useful accessibility information at the following sites:
Disabled Toilets
Access to all disabled toilets throughout Jersey is by use of a RADAR key. They are available for hire from the Town Hall in St Helier, Sand Street Car Park office or from Shopmobility in the lower Sand Street car park. A refundable deposit is required.
Changing Places Toilets
Website for Changing Places Toilets.
Alcohol - coming soon!
Emotional Support
At every stage of your cancer experience emotional support is available in a variety of different forms.
In a Crisis
If you find yourself in crisis please contact your GP or the Samaritans.
For out of hours GP services contact JDOC.
For the Samaritans.
It can be very useful to keep the numbers for these organisations in your phone so that they are readily accessible should you need them.
Face to Face
For Face to Face support we thoroughly recommend Macmillan Cancer Support Jersey. They offer emotional support and counselling.
We also recommend the Listening Lounge for counselling.
Online
In January 2025 the Centre for Psychosocial Research in Cancer (CentRIC+), part of the University of Southampton, launched a fantastic website to guide people through emotional support at every stage of their cancer experience.
CAN-EMPOWER ™
Please note that the links for support are all UK-based. Should you require support here in Jersey you can find local options mentioned throughout our site.
Exercise - coming soon!
Food & Drink
Some cancer treatments change your perception of taste and smell. You may also find that some foods you normally enjoy now have an unpleasant texture to them. It is important to eat and drink to maintain your strength while on treatment. Some tips for doing this are below.
- Try and stock up before starting treatment. You don't know how up to shopping you will feel once treatment starts.
- Until you settle into treatment and know how you feel it is useful to keep stock of some dry foods; bland foods; strong-flavoured foods and some drinkable foods (e.g. soup).
- Stocking plain ice lollies can be useful in case you find it difficult to keep fluids down.
- Hunger can make feelings of nausea worse. Eating little but often can help prevent this.
- If you want to, and can, maintain a healthy diet while undergoing treatment that fantastic. But don't waste any energy on stress if you can't. It's more important that you are getting some food and fluids into you.
- If you are really struggling to eat you might want to speak to your oncologist about getting help from the Dietetics Department. Macmillan Jersey also have a Dietitian you could speak to.
- If you have a history of eating disorders then some of the food issues cancer treatment raises might be particularly difficult for you. It is really important to speak to someone about this. Your Oncologist or GP should be able to refer you for appropriate mental health support. You will already know that one of the best tactics for these kinds of problems is nipping them in the bud.
'Go Bag'
When you are on cancer treatment any symptom or side effect you experience is treated more cautiously by medical professionals. This can mean that you are admitted to hospital having only attended for a routine appointment. Or, if you phone the 'nurse on-call' line out of hours, you may be asked to go to A&E and end up being admitted overnight.
Getting other people to bring you in the right items can be a nuisance but you can get around this by having a 'go bag' ready. Some things you might want to consider keeping in it are:
- medication you take regularly;
- Kindle/iPad for reading or internet access;
- spare chargers for phones/Kindles etc.;
- headphones;
- spare set of underwear;
- eye mask (to block out light);
- ear plugs (the hoovering starts very early);
- toothbrush and toothpaste;
- make-up remover and cotton pads;
- small amount of cash;
- Chemotherapy Record Booklet (if applicable).
Loneliness
No matter how many loved ones you have to support you, cancer can still be a very lonely disease. You probably know people who have had cancer but it can be helpful to make contact with people who are going through it at the same time.
Talking to other people with cancer can be very useful as well as being a good laugh. It allows you a break from explaining to others what is happening with your treatment etc. and allows you to talk about every day subjects.
Local charities may provide social groups where you could meet people. Alternatively, there are a number of forums on charity websites and on social media. Sadly some forums can do more harm than good. It is best to choose a moderated forum hosted by a reputable UK cancer charity.
Cancer Research UK have a large chat forum. It is very well-moderated by a team of nurses. It is open to people living in Jersey.
Macmillan UK have an online community online community. It includes an 'Ask an expert' section.
Both forums are open to those with cancer, their loved ones, and people worried that they might have cancer.
Medical Records - coming soon!
Mental Wellbeing - coming soon!
Mobility Aids
Cancer patients sometimes require mobility aids to get around. This need can be temporary or permanent.
There are a number of organisations in Jersey that can help in this regard:
Another site that people may find useful is Jersey Disabled Travel.
Mortality
As a cancer patient it is normal to ponder your mortality. This is normal even among those whose cancers are curable.
It is often said that British people, in particular, have difficulty discussing death. This leads to people not sorting out their affairs, arranging their own funerals etc.
There are three options that all humans have:
- sorting out their affairs while well;
- sorting out their affairs while ill;
- leaving it to be done by someone who is grieving.
The easiest of those options is the first one.
Some of our tip contributors considered diagnosis a good prompt to put their affairs in order. All they have to do now is amend them if there are any relevant changes in their lives. Should there come a time when they find out they are dying, they will have more time to focus on loved ones. The bulk of the life admin will already be done.
Other Health Problems - coming soon!
Palliative Care
Some people fear the phrase "palliative care". Their only knowledge of it might be Hospice care for those close to the end of their life. Yet the word "palliative" comes from the medieval Latin word for "to cloak". This is a very good descriptor for what palliative care is about. Below are some bullet points on palliative care.
- Palliative care is for anyone with a serious, or life-threatening, illness. It is not just for those close to the end of their life.
- The aim of palliative care is to improve the quality of life of people with serious, or life-threatening, illnesses.
- It can make an illness easier for the patient to bear by tackling pain and other symptoms and side effects.
- It is not just available in Hospices. A Palliative Care doctor is available in Jersey General Hospital.
Relationships - coming soon!
Survival Rates
Just as it can be very tempting to consult "Dr. Google" some people will inevitably search for the survival rates for their type of cancer.
It is very important to remember that any published survival rates you find are already out of date. Those rates also often cover a vast range of age-groups and other variables. Since the study that produced those rates began, cancer treatment has developed at a rapid rate and still every year there are new products coming to the market.
Published survival rates may help you make the change to living each day, having a good quality of life, or sorting out your affairs, but that is all they can offer. If you do look at them please do not put too much faith in them.
Travel Insurance
Travel Insurance for Pre-Existing Medical Conditions
Getting travel insurance when you have a pre-existing medical condition can be something of a nightmare. This section aims to make it a little easier and to raise some points for consideration.
The most important thing to remember is that what matters is what is on your medical records. Patients, especially when dealing with cancer, can make mistakes about what they were told by medical professionals.
Preparation for starting your search
- go through all the 'update letters' sent out by your medical team
- list all medical conditions that you have (inc. high blood pressure, depression etc.)
- list all medications that you take (inc. treatments given at the hospital)
- list all surgeries that you have had in recent years and their dates
- list all admissions to hospital that you have had in recent years
Having all this information together and checking it over helps ensure you don't accidentally mislead an insurer and, because of that, invalidate your insurance.
Two things to consider
- have any tests been undertaken for which you are still awaiting the results?
- are you awaiting diagnosis for any symptom or issue?
If you answer "yes" to either of the questions above then write down as much as you know about the issue, including the types of tests carried out. Unfortunately some tests and potential diagnoses can mean you will be ineligible for insurance cover. This is true even though it is possible to find cover for most medical conditions.
Struggling with the above lists or questions?
If in doubt about any of the above you may want to speak to the hospital about viewing your medical records. You can try and clarify some issues with your medical team but, understandably, they may not be keen to put anything extra in writing and might direct you back to the update letters.
Completing the insurance application
Complete the form considering how you will fight your case if your claim is challenged. Things that help with this are:
- if you counter a difficult or ambiguous question ask the insurer what they mean;
- when you do answer the difficult/ambiguous question take note of your reasoning;
- keep all the lists you've created, and other documentation, together.
Final Considerations
- If you are holidaying in the UK remember the reciprocal health agreement only covers certain things, ensure you read it before relying on it.
- If you have any medical changes (good or bad) before your trip starts you must let your insurer know.
- Do you have a credit card, or access to a method of payment, to cover medical care should your insurer try to challenge your claim?
As already stated the system is designed to pay out. If you have completed the application to the best of your knowledge then you have done all you can. Any refusal to pay out should be fought even if you have made a genuine error, and that's where keeping all your notes and a record of your reasoning together could be helpful.
Really Important
If you need to make a claim on your travel insurance the insurer will specifically look for issues with your policy that could invalidate it. For most cancer patients they are taking out this specialist insurance because of their cancer. However, any errors in other parts of their declaration could cause the policy to be voided. So it is really important to be truthful to the best of your knowledge and that means pulling together all information you have access to.
Contrary to popular belief insurers are not looking to catch you out or to cheat you. However, there are people who intentionally try to cheat the system so insurers have to protect themselves. The system is designed to pay out, at least partially, where the applicant has completed the application to the best of their knowledge.
Help Finding Cover
The UK Government website Money Helper has a directory of companies that provide Travel Insurance for pre-existing medical conditions. Their directory can be found here. N.B. This is a UK site for UK residents. Some of the companies listed will provide insurance cover for Jersey residents but others won't.
Insurance Companies That Cover Jersey Residents
As at June 2023 there are two companies that Lorna knows have provided cover for a Jersey resident in recent days. These are listed simply to help with your search.
Please be aware that:
- Inclusion in this list is not a recommendation for the company;
- any of the companies listed could cease providing cover for Jersey residents at any time.
If we become aware of other companies having recently provided cover for Jersey residents this list will be updated accordingly.
Travel (local) - coming soon!
Working With Cancer - coming soon!
Intimacy - coming soon!
Emotional Support
Please be aware that organisations that give emotional support to patients often also support family and carers. We offer some useful links below.
In a Crisis
If you find yourself in crisis please contact your GP or the Samaritans.
For out of hours GP services contact JDOC.
For the Samaritans.
It can be very useful to keep the numbers for these organisations in your phone so that they are readily accessible should you need them.
Face to Face
For Face to Face support we thoroughly recommend Macmillan Cancer Support Jersey. They offer emotional support and counselling.
We also recommend the Listening Lounge for counselling.
Online
In January 2025 the Centre for Psychosocial Research in Cancer (CentRIC+), part of the University of Southampton, launched a fantastic website to guide people through emotional support at every stage of their cancer experience.
CAN-EMPOWER ™
Please note that the links for support are all UK-based. Should you require support here in Jersey you can find local options mentioned throughout our site.
Self-Care
N.B. Most people donate to cancer charities at some point in their lifetime. And they do so because they want the support to be there for people in their time of need. If you are now the one in need please take the support, others donated so it would be there for you!
It can surprise people to find out how the news of a loved one's cancer affects them. It might drag up old experiences of a loved one who had cancer. Some find themselves grieving again for a loved one they lost years ago. Others feel lost because this isn't a situation they can fix.
Patients are grateful that people want to help and support them. But, it mustn't come at the cost of their own well-being. Please be aware of how the news is affecting you. Be aware of your own mental health. If you need to talk to someone then please do.
There are a couple of things it is worth remembering.
- Your loved one doesn't need you to be anyone other than yourself. They don't need you to fix things for them. They need you to be the person you've always been. And they need you to take care of yourself.
- Suffering isn't a competition. Something cancer patients hear a lot is "but it isn't as bad as what you're going through". It can be frustrating.
Everyone's life and pressures are different. People's ability to cope with situations varies. If the person with cancer is someone who has supported you over the years, they will still want to support you. With fatigue, in particular, they may not be able to support you in the same way as before. But they will usually still want the opportunity to support you in your difficulties.
If in doubt, ask them! Please don't shut them out of supporting you if it's something they want to do. Relationships are still two-way.
Supporting Your Loved One
Still The Same Person
The best bit of advice we can give to a loved one of someone with cancer is to just be there for them.
You know them, you know their interests and what makes them laugh. They are still that person and will need those interests and to have a laugh. Cancer is an illness that they have, it doesn't define them (even if it does sometimes feel like it)!
It is totally understandable that when you speak to them you will ask how they are. And the assumption will be that you are asking about the cancer. So you might also want to ask specifically about other aspects of their life. Maybe about how they are getting on with study, or a hobby, for instance. It's easy for the patient to almost get lost in the cancer. Knowing that people still see other aspects of them can be really helpful.
Emotional Rollercoaster
The physical side of cancer can be hard for a patient. Most people have some idea of the kinds of things it can entail.
But until someone gets cancer, they have no idea of the emotional rollercoaster it brings. And that will affect their loved ones.
Here are some things it might help to be aware of.
- Your loved one may feel guilty about having cancer. They may worry about what they are "putting you through". It's irrational. They shouldn't feel that way. But it is also quite normal. Be aware that they may be dealing with this on top of their emotions about what is happening to them.
- "Scanxiety" is a word in the cancer community. No-one seems to get away from it. Scans become so normal that the patient isn't always aware of their anxiety. It can present in subtle ways. They may just be more 'on edge' than usual. And so you may need to be more patient. The days leading up to the scan and while waiting for the results seem to be the most anxiety-inducing days.
- Good news should be good news. But with cancer it is rarely that simple. Don't be surprised if your loved one has mixed emotions when receiving good news. They may need time to come to terms with it, just as they did with bad news. Life has changed for them in a major way in a short space of time. Any kind of news takes a toll.
Might you be ill?
Are you carrying a virus or infection?
Cancer patients are partly reliant on others to help protect their health.
Vaccinations are sometimes less effective in cancer patients because of their treatment. Their loved ones being vaccinated can increase their protection from disease.
Another issue is if a cancer patient develops an infection or virus it might delay their cancer treatment. That can negatively affect their prognosis.
Cancer patients need their friends and family, but they also need to avoid infections and viruses. So before spending time with a cancer patient there are some questions we advise considering.
- Might I be carrying a virus or infection that is transmitted by touch or through the air?
- Do I have any symptoms that could be indicative of a virus or infection?
- Does a friend or colleague I've been around have a virus or infection?
If the answer to any of these questions is yes then you might want to consider the following.
- If the cancer patient is in your household consider how the virus or infection spreads. You may need to increase your hygiene measures; limit contact; ventilate rooms well.
- If the cancer patient lives elsewhere consider whether they need you to visit. Or whether you could catch-up virtually. If they do need a visit then consider how the virus or infection spreads. You could take more care over hygiene; wear a face covering etc.
- If it's nice weather it may be best to see your loved one outdoors.
It is worth remaining aware that illnesses your body can shrug off could be life-threatening for a cancer patient.
Language Matters
Militaristic Language
Militaristic language is common when discussing cancer. It is used in two distinct ways:
- in government and charity campaigns around society fighting these diseases by finding cures;
- when talking to a cancer patient about their own cancer.
There is some evidence that the first use can be problematic. Some studies show that use of militaristic language in this way can discourage people from taking steps to reduce their risk of cancer.
However, the second use is particularly problematic and upsets many (but not all) cancer patients.
When someone dies of cancer we read, or hear, that they "lost their fight" with cancer. The wording suggests they either didn't fight hard enough, weren't strong enough, or didn't have the right attitude. They were partly to blame for their death. Yet none of that is true. They died because their specific cancer didn't respond to treatment as well as other people's cancers did.
Cancer patients often hear "you can fight this" or similar. It is even said to people who are incurable. What message does that send to someone when their time comes?
At cancer.JE we recommend avoiding this kind of language unless you have checked with the cancer patient how they feel about it. It can lead to the patient feeling like they have failed or are failing.
Positivity
Cancer patients are often told to "stay positive". Yet positivity is not a cure for cancer.
Positivity can help people deal with symptoms of cancer and side effects of treatment. But it cannot cure anyone.
Cancer patients are coming under increasing pressure to appear positive. If someone is naturally a positive person then that's fine. But faking positivity takes its toll on a person's health.
Even the most positive cancer patient will have rough days. If someone has told them to be positive they might feel unable to approach that person when they are struggling.
Information on Cancer
Please see our section titled "Information on Cancer" within the Newly Diagnosed section.
Cancer Patient Fatigue
Both cancer and its treatments can cause fatigue. This is a very different sensation to what people experience if they've 'overdone it'. It's also different to how people feel when they say they're exhausted.
Your loved one could be excited for a long-awaited catch-up with you. But within minutes be so wiped out as to no longer be aware of what's going on. For the person with cancer the fatigue can seem to flood their body very quickly. They will be happily chatting. Then minutes later realise they are no longer able to take in anything that's being said.
Please don't take offence if this happens. It's not you! They can't choose to perk up and keep chatting. The fatigue is so strong some will say they need to go for a sleep. But others might worry about appearing rude. Especially if they know they won't be able to see you for some time.
Fatigue can last long after a patient has been given the 'all-clear' from their cancer.
Vaccinations
Some cancer patients are at increased risk from viruses. Common viruses that others shrug off can cause severe harm, or even death, to a cancer patient. Their level of risk often depends on their treatment.
Your loved one may be advised to receive certain vaccinations. Whatever your views on vaccination please do not interfere. If their Oncologist advises vaccination that advice is based on many years, even decades, of training and experience. It is also based on deep knowledge and understanding of your loved one's cancer.
Vaccinations are sometimes less effective for cancer patients. Effectiveness varies according to their type of treatment. So they still need to be cautious, even when vaccinated.
Please also see the section "Might you be ill?"
Dying With Cancer
While many cancer patients will receive the 'all clear' at some point, unfortunately this isn't the case for everyone. Some people will reach the point where there are no (or no more) surgical or treatment options for their cancer.
This is exceptionally difficult news to hear and there is no right way to handle such information.
Support is available for patients and their loved ones through:
N.B. The last two organisations are UK charities. While they will be able to give general advice the Laws across the UK countries may differ from those in Jersey. Should you require general legal advice please see our Experts' Corner section in the first instance. For advice specific to your situation please contact a local lawyer.
End-of-Life Care
As well as the hospital, there are two organisations in Jersey that provide end-of-life care.
These are:
Practicalities
Many adults put off matters which they associate with death, such as:
If you haven't previously considered the legal aspects relating to death then reading Simon Lofthouse's overview in our Experts' Corner would be a good place to start. Please note that Simon also offers a free basic Will-writing service to anyone who contacts him through cancer.JE. Should you wish to make use of this service please contact us by email.
More information and support can be found at Compassion In Dying. It is important to note, however, that this is a UK organisation and so any legal advice they give will pertain to Scottish Law, English and Welsh Law, or the Law in Northern Ireland. This will likely differ from Jersey Law but some of the considerations they mention will still apply so their site could still be helpful to you.
End-of-Life Choices
The choices that people have at the end of their life in Jersey are limited.
On their website Compassion In Dying have information on matters you may wish to consider. Please be aware that the various Laws across the UK countries could differ to the Law here in Jersey.
Assisted Dying is not currently legal in Jersey although it is expected that it will be legal in the coming years. You can find out more about the matter here.